Since the hormone of the corpus luteum is responsible for the preparation of the womb lining after ovulation, a luteal phase defect can be the reason why the desire to have children has not yet been fulfilled.1 This article provides a comprehensive overview of the causes, symptoms, consequences and possible course for action.
Was Du auf dieser Seite findest:
What is a Luteal Phase Defect?
After ovulation, the so-called corpus luteum is formed in one of the woman’s two ovaries. It’s called that because its tissue is actually yellow. The task of the corpus luteum is to produce progesterone. This is one of a woman’s most important sexual hormones.
Progesterone
The corpus luteum hormone is a female sex hormone and is formed as natural progesterone after ovulation by the corpus luteum. While in the first phase of the cycle the mucous membrane of the uterus grows under the influence of the hormone oestrogen, the task of the corpus luteum hormone is to prepare the endometrium for implantation of the fertilised egg.
If the ovaries produce too little progesterone and the corpus luteum is insufficiently formed, this is referred to as luteal phase defect, luteal insufficiency or corpus luteum insufficiency.2 If you suffer from a progesterone deficiency, there may be a deficiency in the subsequent hormones that are produced with the help of progesterone. The other hormones that play a role in the women’s cycle and how they change over the course of the cycle are listed in our guide section. Here you will find everything about the effects of the various hormones in the female menstrual cycle.
What are the Symptoms of a Luteal Phase Defect?
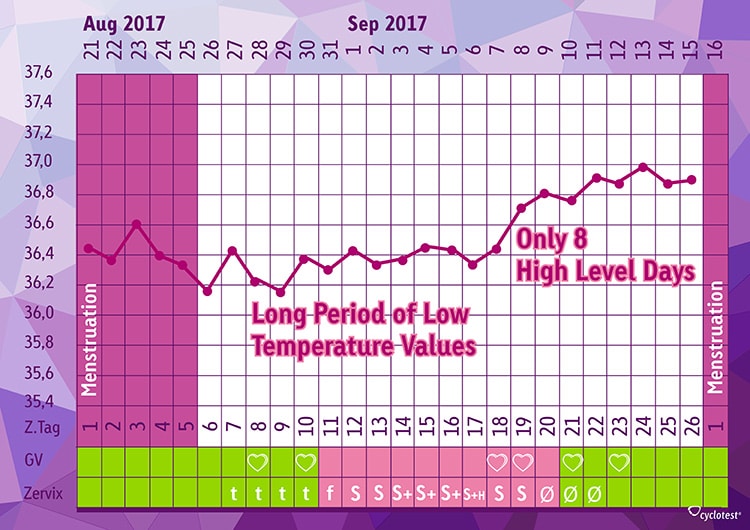
An irregular cycle can be the result of a luteal phase defect. In most cases, a shortened second cycle phase – i.e. the phase after ovulation, also known as the corpus luteum phase – can be detected while ovulation takes place regularly. The shortened second half of the cycle has less than 8 to 10 elevated temperature values.1 The blood level of the corpus luteum hormone can also give an indication of a possible luteal insufficiency if it is too low in the second phase of the cycle.3
The above picture shows a 26-day cycle with a shortened phase after ovulation. The ovulation date was determined by measuring the waking temperature. The corpus luteum phase starts with the first comparatively elevated temperature value on day 19. This so-called elevation continues in this example until the end of the cycle on day 26.
As this example shows, measuring your body temperature can provide interesting information on the symptoms of a progesterone deficiency. Since the temperature is measured in the morning before any activity, we speak of basal body temperature in this context. As already described, it usually increases after ovulation and remains at this elevated level until the next menstrual period. What is important is that we are talking about only a few tenths of a degree, which characterise these high level days.
If this ascent to the upper range is rather “stair-like”, i. e. progressively increasing, this can also be a symptom of progesterone deficiency.4 Mid-cycle bleeding or spotting in the second phase of the cycle are also symptoms of progesterone deficiency.1
Further indications can be previous miscarriages, but also general symptoms. These include muscle and joint pain, myomas in the uterus, cysts or a weakness of the bladder, as well as symptoms due to the premenstrual syndrome (PMS). These symptoms are often not associated with a luteal insufficiency, but may indicate it.2
What are the Causes?
The corpus luteum must be fully produced in order to perform its important functions. The reasons for a disorder of the corpus luteum with a high temperature level of less than 10 days are manifold. Previous infections may have damaged the ovaries. Other causes can also be functional disorders of the adrenal gland, thyroid gland and pancreas (diabetes), which can have a negative effect on the production of the corpus luteum in the ovaries.
Furthermore, the causes can also be located in the intestine, where chronic irritation caused by vitamin and mineral loss can lead to a reduced ovarian function. Ovarian insufficiency is also a possible cause where the pituitary gland does not release the hormones FSH and LH sufficiently, which means that the ovaries are not stimulated enough. The onset of menopause is often characterized by progesterone deficiency. Finally, environmental pollution can also have a negative impact on the activity of the ovaries.
What are the consequences of a lutal phase defect?
Progesterone is crucial for a successful pregnancy. If this hormone is not sufficiently produced, problems may arise during implantation of the fertilised egg and subsequently during pregnancy. The most important function of progesterone is to maintain pregnancy during the first weeks. The corpus luteum hormone, for example, provides the womb lining with nutrients that allow the egg to mature. Finally, a lack of progesterone can lead to an early termination of pregnancy if the hormonal conditions are inadequate.
Furthermore, the hormone prepares the mammary gland for milk production. Finally, progesterone ensures that no further egg cells can nest and prevents the eggs from maturing in the other ovary. A lack of progesterone is not an independent disease, but rather a functional disorder of the ovaries, in which no complete corpus luteum can be formed as a result.
Luteal Phase Defect – What really Helps
If your desire to have baby remains unfulfilled, it is advisable to consult a doctor. If you have already observed your cycle and maybe even documented your basal body temperature, this can provide important clues. Further medical examinations can then be arranged by your doctor in order to achieve a successful pregnancy. It is helpful to look at your cycle history over a longer period of time, because a single cycle during which there may have been a luteal insufficiency in the second half of the cycle does not necessarily has to be proof that this applies to each cycle. It can also be determined whether ovulation takes place at all.
cyclotest myWay provides important information on a possible progesterone deficiency.
The cyclotest myWay cycle computer can provide you with fundamental support: On the one hand, the cycle length is determined by regularly entering the start of menstruation. On the other hand, measuring the basal body temperature in the morning illustrates the course of the measured values in the form of a graph. This makes it easier to detect stair-like ascents. If the cycle computer detects irregularities that indicate such a disruption, an indication of a possible luteal insufficiency appears on the display. This note may save valuable time. In addition, the cycle graphs of past cycles can be read out and printed using the corresponding software – a great basis for an appointment with the gynaecologist.
How Do I Get Pregnant Despite a Luteal Phase Defect?
Usually, the high altitude lasts 10 to 16 days before the next menstruation begins. If you find that the high level days of each of your cycles is too short (< 10 days), talk to your gynaecologist and inform him/her about your cycle observations. As a treatment, stimulation of the follicle is recommended. This refers to a hormonal treatment (usually in the second half of the menstrual cycle), which contributes to an improved corpus luteum function.1 Individual diagnosis and appropriate, usually hormonal, treatment is initiated by your doctor, for example with clomiphene.
Vitex Agnus-Castus to Treat Luteal Insufficiency
Since antiquity, Vitex agnus-castus has been valued as a medicinal plant: the intake of Vitex agnus-castus is said to help improve a luteal phase defect. Smaller studies have shown that the active substances from the seeds harmonize the female hormone balance and have a positive influence on fertility.5,6 The luteal hormone controls the structure of the uterine lining. The Vitex agnus-castus stimulates the body’s own progesterone formation in the corpus luteum phase. In addition, Vitex agnus-castus counteracts an increase in prolactin levels. Prolactin inhibits the production of various hormones that are important for fertilization. The researchers of the studies conclude from their results that Vitex agnus-castus can be a useful supplement to conventional therapies or an alternative.
Going off the pill and Luteal Phase Defect
Many women who wish to have a baby used the contraceptive pill. After stopping the pill, menstrual cycle irregularities occur in many cases. These include shortened cycles, prolonged cycles, cycles without ovulation and cycles with luteal insufficiency. A study revealed that a luteal phase defect can increase up to the 7th cycle.7 Here it is helpful to observe your cycle, to document your ovulation and to detect disturbances in the second half of the cycle. Most menstrual disorders are self-regulating and no special treatment is necessary. However, for women who wish to have a baby this may mean that it takes longer after stopping the pill than for women who have not taken the pill at all.
What examinations follow if there is suspicion of Luteal Phase Defect?
The expert for gynaecology, Prof. Dr. Ingrid Gerhard, answers:

Prof. Dr. Ingrid Gerhard
Sources:
1 Madejski, M.: Das alternative Kinderwunschbuch – Die besten Naturheilkonzepte für die Fruchtbarkeit. 1st edition. Munich 2015.
2 Raith-Paula, E. et al.: Natürliche Familienplanung heute. Modernes Zykluswissen für Beratung und Anwendung. 5th edition. Heidelberg 2013.
3 Schmidt-Matthiesen, H. und Wallwiener, D. (Hrsg.): Gynäkologie und Geburtshilfe. 10th edition. Stuttgart 2005.
4 Jürgensen, O. (Hrsg.): Hyperprolaktinämie-Prolaktinome. Physiologie – Klinik – Therapie. Berlin 1988.
5 Bergmann, J. S.: Die Wirksamkeit des Komplexmittels Phyto Hypophyson L bei weiblicher, hormonell bedingter Sterilität – Eine randomisierte Doppelblindstudie. heiDOK. 2001.
6 Westphal, L. M. et al.: Double-blind, placebo-controlled study of Fertilityblend: a nutritional supplement for improving fertility in women. Clin Exp Obstet Gynecol. 33(4):205-208. 2006.
7 Frank-Herrmann, P. et al.: Zyklusverhalten nach Absetzen von oralen Kontrazeptiva. J Reproduktionsmed Endokrinol. 2006.